Priority: Protect physician autonomy and keep nonmedical entities from interfering with patient care, particularly amid health care consolidation.
Background: In an increasingly consolidated health care market, physicians like Tony Aventa, MD, are finding themselves challenged to stay viable so patients can have health care options they trust.
In line with national trends, data from a Physicians Advocacy Institute/Avalere Health study shows 73% of Texas physicians were employed at the start of 2024, with nearly 42% employed by hospitals and hospital systems and nearly 31% employed by other corporate entities.
“It’s pretty black and white; [some] physicians can’t keep their practices open,” Dr. Aventa said. “They’re struggling to find legitimate partners to work with, and when they can’t, unfortunately, they can potentially be taken advantage of in a way that might sacrifice patient care.”
As an Austin primary care physician in a practice that’s operated for 90 years, Dr. Aventa says payment-related financial challenges led them to focus on outpatient care, letting hospitalists manage care whenever patients required hospitalization.
“Obviously, that changed the dynamics between [us and] our patients,” he said. “They were expecting to see us in the hospital. That was a difficult decision at the time.”
But his group found that setup preferable to the risks of entering into an arrangement with a profit-minded investor whose cost-cutting decisions also might lead to greater physician burnout.
Dallas cardiologist Rick Snyder, MD, fortunately found a way to grow his current practice utilizing a private equity model that is physician-led, “which allows us to stay independent of hospitals and corporate models and embrace low-cost sites of service and value-based reimbursement models that cut the cost of care,” he said. “In our model, we’re capturing some of those savings. This is why independent investors are interested. Hospitals and corporations use capital to grow. We do too, we’re just accessing it a different way.”
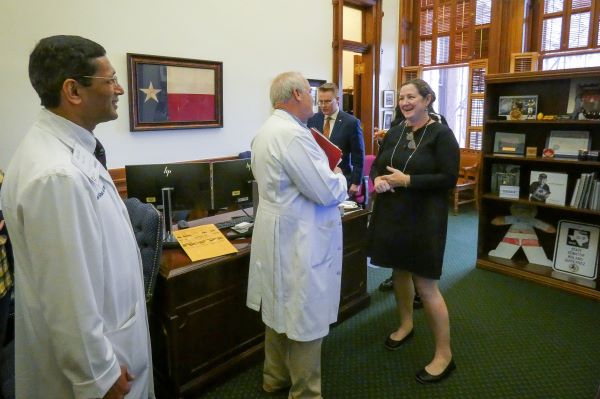
TMA Council on Socioeconomics member Sherif Zaafran, MD, is a partner in a practice that similarly attracted private equity investment and negotiated a structure maintaining physician independence for their practice.
“It’s absolutely critical that clinical autonomy, regardless of what kind of financial or corporate structure is out there, is maintained. Decisions affecting local practices must be made by the physician or a board of physicians,” to ensure patients’ interests come first, he cautioned. “Vertical integration is actually happening more in the insurance side, and as it's becoming more and more ingrained in our health care system, I feel like we do have to make sure that we safeguard physician autonomy and practice sustainability.”
A November 2024 U.S. Government Accountability Office report confirmed that health insurance market consolidation is on the rise, including in Texas, saying “a concentrated health insurance market may indicate less issuer competition and could affect consumers’ choices of issuers and the premiums they pay for insurance.”
Solutions: Whatever the practice setting, TMA will work this session to help ensure physicians can exercise professional medical judgment in treating patients without financial or other outside pressures. Texas corporate practice of medicine laws offer those protections by prohibiting lay corporations from practicing medicine or employing physicians to provide professional medical services (with some exceptions).
TMA will work to safeguard those laws.
“Texas is to be applauded because we’re very mindful of protecting physicians and not allowing the corporate practice of medicine,” said Lane Schnell, MD, an emergency medicine physician with the UT Health East Texas system in Tyler who has experienced both employee and independent contractor relationships with hospitals.
Dr. Schnell suggests some arrangements between medicine and corporations can both adhere to the doctrine and financially support practices, provided they exhibit “sound business principles and ethics coupled with good health care ethics.”
TMA generally anticipates defending against insurer-supported bills either providing for consolidation of physician practices or bolstering vertical integration and specifically expects a bill creating a process for reviewing health care mergers and acquisitions.
“The idea would be to add some kind of a state check against health care consolidation,” said Ben Wright, TMA director of public affairs. “That bill would include private equity and include a transparency of ownership provision.”
Such transparency is especially relevant in an era in which, as TMA Associate Vice President of Public Affairs Michelle Romero points out, health care is a sought-after industry for private equity investors.
“We stand ready to protect medicine against any of these challenges,” she said.
TMA’s Top 10 Priorities for the 2025 Legislative Session
Phil West
Associate Editor
(512) 370-1394
phil.west[at]texmed[dot]org

Phil West is a writer and editor whose publications include the Los Angeles Times, Seattle Times, Austin American-Statesman, and San Antonio Express-News. He earned a BA in journalism from the University of Washington and an MFA from the University of Texas at Austin’s James A. Michener Center for Writers. He lives in Austin with his wife, children, and a trio of free-spirited dogs.